“I still have a way to go before I can sit in a hair salon and not blur my eyes in front of the mirror; however, I no longer stress over bad hair days, I just swish my glasses into the hairband position.”
Once an impossible dream, here I am lounging outside in the midday sun.
I’ve not checked the mirror today, though I’m not quite bare-faced because I’m still wearing yesterday’s makeup. I haven’t gotten so far in my recovery that I can just grin and bear it all. Day-old makeup is a step in my desensitisation process. Still, I’m acutely aware that someone could stroll up the path and see me raw.
My husband approaches and I fight the instinct to shrink away. Instead of increasing facial camouflage, I slip my glasses up to form a hairband. This is not entirely innocent, rather a reconfiguration because I’m covertly concealing my hair parting. My hands jerk to cover my face, though I keep them on my book until the sensation fades.
Seven years ago, four layers of window-dressing shrouded me in perpetual darkness. Facing daylight demanded days of preparation, fighting through rituals, as I struggled to make my face publicly acceptable. I would wash and reapply makeup until my skin burned, rendering me housebound and without groceries for yet another day.
At the height of my struggle, I wore sunglasses until friction blistered my nose and ears, their arms hooked on for dear life. Even those lesions became part of my camouflage, a temporary deformity I rationalised as diverting attention from my perceived imperfections. But instead, BDD was trying to manifest itself in physical ways, to prove, look, I am deformed.
When at my local Sainsbury’s, the security guard asked, “Why the sunglasses indoors?” I replied with a rehearsed excuse, “I’m recovering from surgery.” Then I avoided that store for a year, driving 45 minutes out of my way for a pint of milk.
After waiting 22 years to “grow out of it,” as my friends assured me I would, I self-prescribed an exposure exercise: a bodybuilding competition, because once I’m lean then I’ll be happy, right?
Over four months, I trained six days a week. Then, during peak week, I chugged 6 litres of water daily and tapered my calories down to 450. I stepped on stage, abs defined, my face thinned out, and I made it into the top ten, only to realise I’d built a body as unhealthy and unsustainable as the pills I popped. My bikini sparkled, my skin glistened, and my stage makeup concealed a dark truth; my lips had turned grey from injecting myself with unregulated tanning agents.
BDD learned to exist on a new frequency, and I judged myself on an unreasonable scale, measuring body fat by the millimetre whilst swallowing dodgy fat burners and diuretics. After I binged my way back to normal, a real medical crisis erupted one morning and sparked a dilemma: Do I call an ambulance or apply makeup?
I imagined the paramedics, revolted by my face, and decided to leave them something nicer to look at. It’s better to be dead wearing makeup than to show my raw face in public.
I wobbled to the bathroom and set out my instruments. If I died doing eyeliner, it would be the most honest way to go.
Stumbling into the GP’s office the following day, the medical form asked, “What is your eye colour?” I had no idea; I hadn’t seen my eyes in daylight in over two decades since I closed my curtains at thirteen. And with nobody to call because I had ghosted myself into reclusivity, I had to guess the answer: blue?
Lacking a proper vocabulary, I shared how I injected myself and took under-the-counter supplements, meanwhile remaining silent about my two-decade mirror obsession because, to me, it was nothing more than a “vanity curse,” my shameful, dirty little secret.
Discovering The Broken Mirror by Dr Katharine Phillips finally put a name to my situation: Body Dysmorphic Disorder (BDD). I was eager to consult Dr Phillips, except she was in America and I was tethered to my mirror in Britain. Even if I could get beyond my pre-travel rituals, flying had become an excess baggage nightmare, requiring me to stow mirrors, lights, and window coverings.
My recovery began with a single decision: to peel away the layers from my windows. Inch by inch, I unravelled the blinds and peeled back the curtains, shielding below a ball cap or behind sunglasses, taking small steps forward and then retreating, until I could finally face myself. All the while, audiobooks, movies, and music distracted my self-criticising voice.
In 2019, I flew to New York to meet Dr Phillips. Her diagnosis gave me new self-awareness, and I came away with a surprising side diagnosis: non-purging bulimia, another bodybuilding souvenir.
Today, I’m happily married and settled in Washington, and my active recovery is structured around these core practices: I restrict my makeup routine to just 15 minutes, and I often glance in the mirror no more than twice a day, occasionally forgetting until evening. I avoid interacting with my reflection when outside my home, hyper-vigilant of every reflective surface. Headphones replace sunglasses, and audiobooks not only provide a distraction, but have given me back my voice.
A year ago, in my journal, I recognised a tone change. I called it “Bogey Maid,” inadvertently giving my BDD a name and separation. Now I turn my scars into stories.
Moments ago, I finally checked my mirror. Close to the window where I can see my blue-grey-green, colour-confused eyes. I recognise my face looks normal, adding another increment towards recovery.
Sitting here right now, the warmth I feel is not a flush of embarrassment or shame, just a friendly kiss from the sun.
Thirty-five years of worrying about my face, chasing superficial fixes, and hiding behind camouflage led to nothing but isolation where I tiptoed near death. But just one inch of daylight led me here, to my husband, my cat, and a life.
I still have a way to go before I can sit in a hair salon and not blur my eyes in front of the mirror; however, I no longer stress over bad hair days, I just swish my glasses into the hairband position.
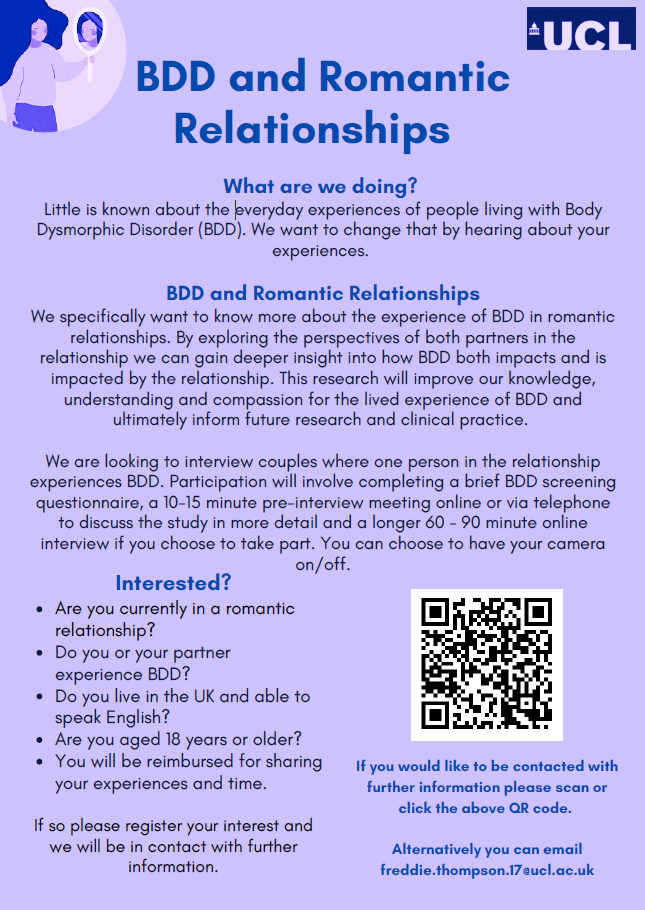
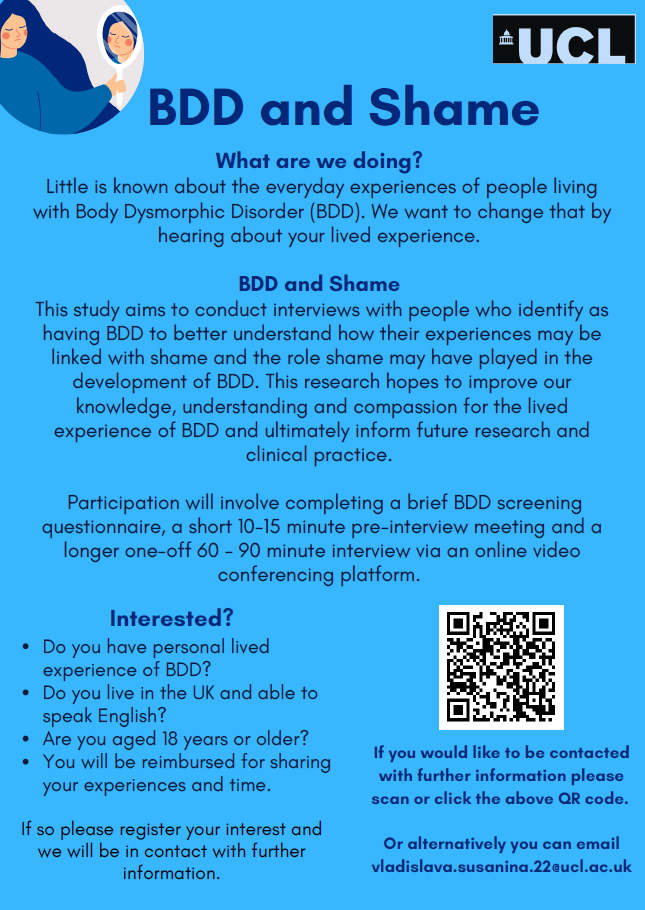
I’m thankful for Dr Phillips, the BDD Foundation, and every researcher who studies and supports those of us living with this not-so-invisible and destructive disorder.
If my experiences sound like they could be your own, or if your feelings seem misaligned with what’s considered typical, don’t delay seeking help as I did. BDD isn’t something you simply outgrow, and it’s not a universal experience. With the right approach and support, freedom awaits you too.
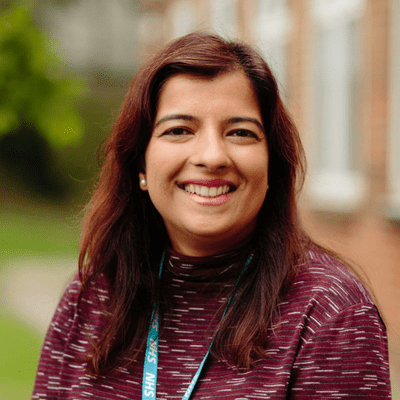
About Carrie-Ellise Poirier…
In 2005, a bidding war on eBay unexpectedly launched Carrie-Ellise Poirier into the literary world.
Having navigated 30 years of Social Anxiety and Body Dysmorphic Disorder, and driven by a relentless pursuit of recovery, Carrie’s life has been a series of unexpected turns, from securing a coveted role as a flight attendant with a premier airline to competing in a bodybuilding contest.
Today, Carrie channels her unusual experiences into her writing, establishing Bogey Maid as her platform for promoting positive body image while finalising her forthcoming coming-of-age memoir.